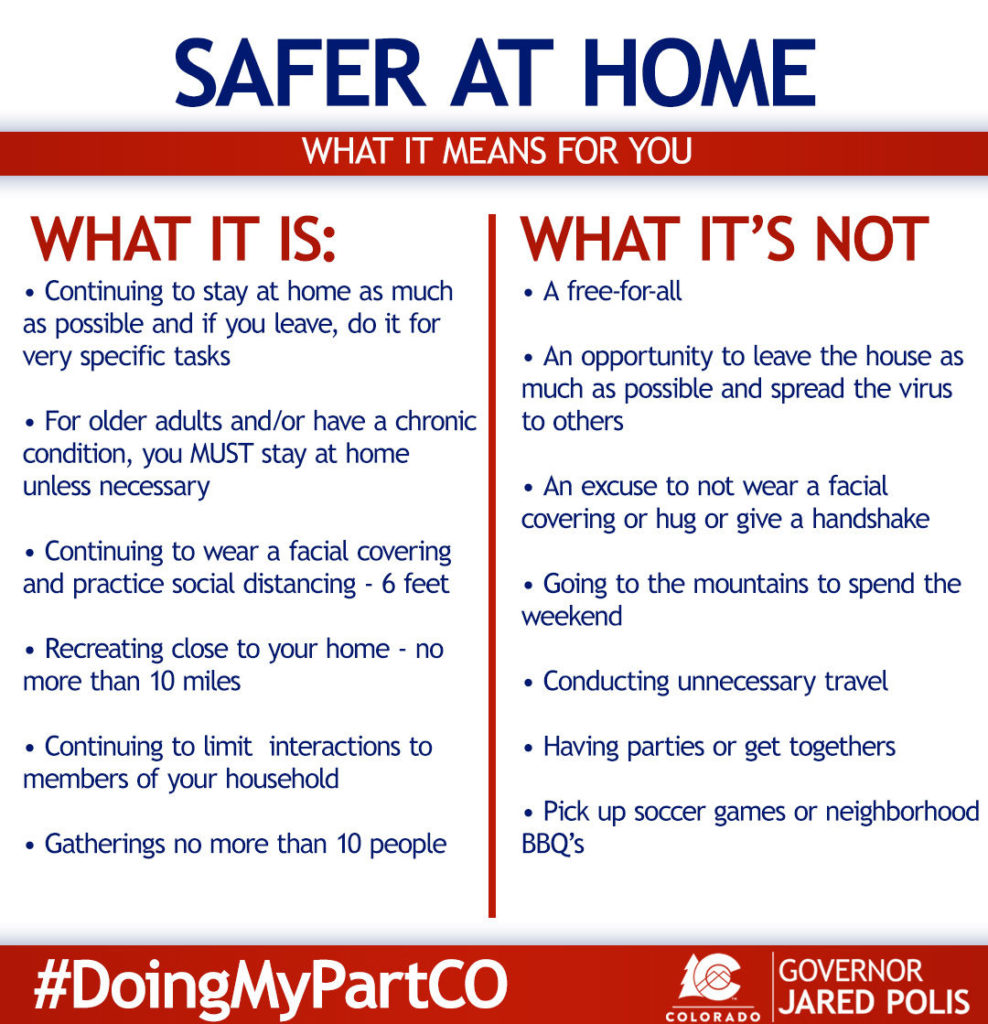
It’s been a week since my first Covid-19 blog on 3/18/20, and I will have to admit how amazed I am at the feedback and attention it got. A LOT has happened since that day, and not all of it has not been so positive. Here in Colorado Governor Jared Polis officially announced today (3/25/20) that ALL residents of Colorado are under a ‘Stay at Home’ order. Meaning we’re supposed to stay in our place of residence with the exception of essential trips (medical, food, work for us exempt jobs) and exercise, all the while maintaining social distancing from anyone not in our immediate household (which is just me and my cat). For many of us this isn’t too much of a change, but for those who didn’t think this was serious it’s probably a bit of a rude awakening. Since my post LAST WEEK (now 3/26/20) the number of worldwide confirmed cases has more than doubled to 530,000 (from 219,243), the number of deaths has increased to over 24,000 (from 8,968) and on 3/26/20 the United States confirmed over 17,000 NEW cases, making us the country with the most confirmed cases in the world (go us?) (worldometers.com, washingtonpost.com).
I’m hoping by now that most people realize how serious this is, and that there is definite need to slow the spread; both to allow our medical care teams to keep up and to allow scientist to keep working (please no arguments on the political actions or economic impact, yes it’s going to be bad). My goal in this blog write up is to outline the things that help us bring this pandemic to an end (or at least slow it down). I’ll be focusing on the status of testing in the US (what those tests are), the current drug pipeline and what is being tested, the process and timeline for a vaccine and whether there’s anything to the claim of seasonality with the infection. So here we go, Round 2, diving back into the Science!
Testing
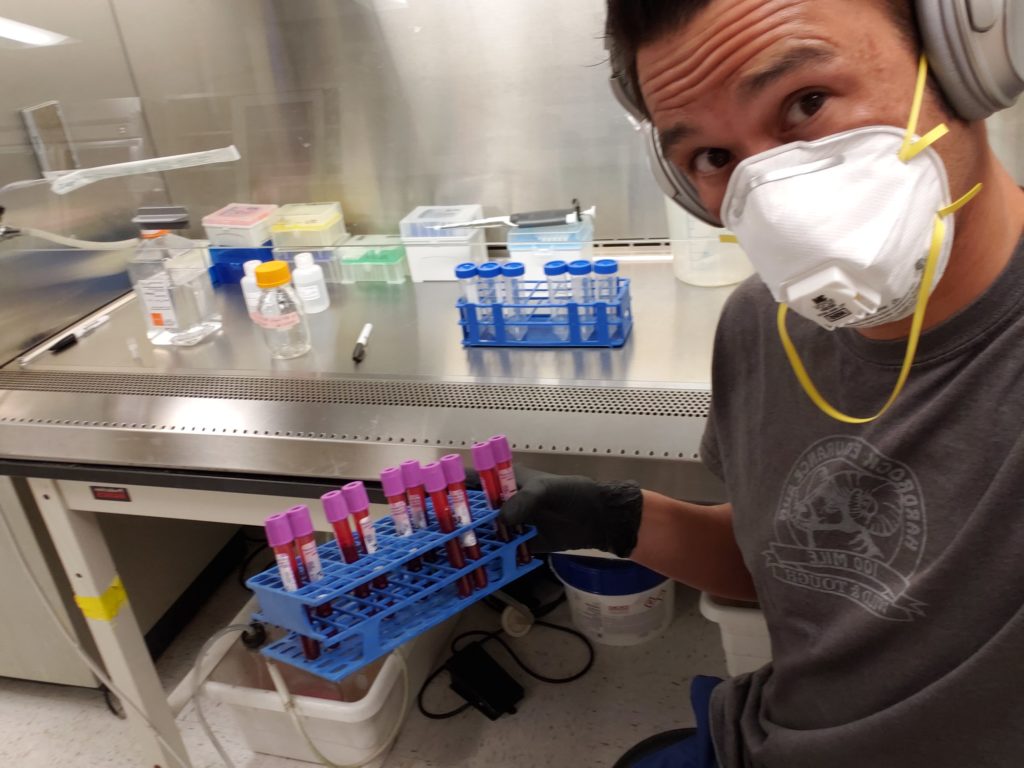
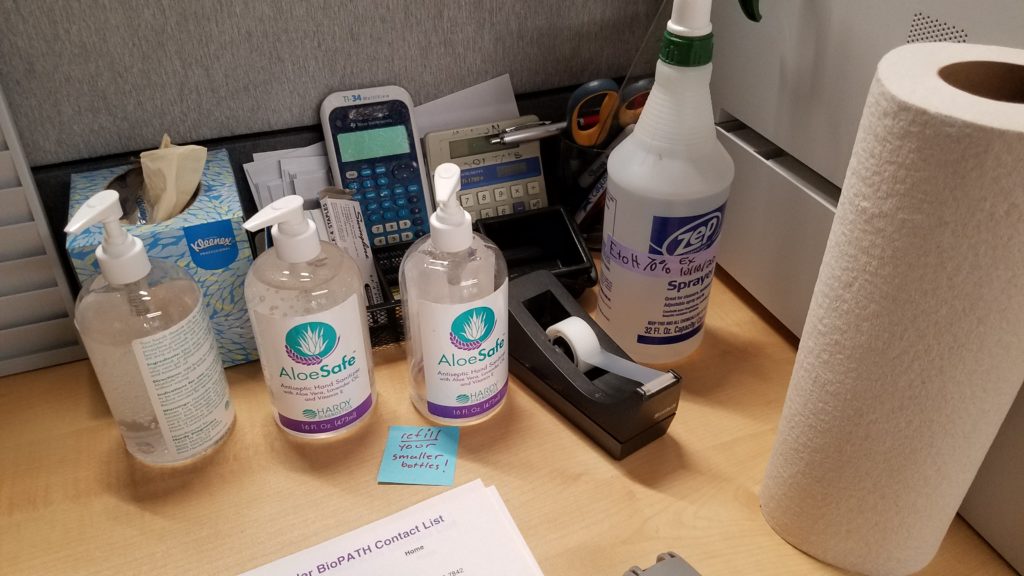
So in my last post I wrote about how much of a mess the Covid-19 testing and surveillance were in the United States, well sadly that has not improved a whole lot. While we’ve definitely tested a lot more people, I’ve been hearing from providers and hospitals all over the country that they’re only testing people who are in high risk populations or have advanced/severe cases of disease. Very recently a rash of new tests have become available to providers and hospitals, meaning the surveillance is starting to grow and hopefully this will continue. There is definitely hope as we are soon to have two different types of tests available, the PCR based tests that we’re currently using for diagnosing active disease and an Antibody based test.
The PCR based test is the one I spoke about previously where labs are able to look for pieces of the viral genome in human samples (usually a nasopharyngeal swab). This test can be quite sensitive and is used to identify infected patients even during the early stage of disease. Though, being such a sensitive test it is more prone to errors and false positives (though they are still very well validated), hence why the original CDC test failed. The other issue right now is that because there’s not a lot of top down coordination in the United States we have dozens of different labs who have created PCR based tests that are being used in different parts of the country. Here are a few of the companies/hospitals who have created PCR based tests; ThermoFisher, Roche, Cepheid, Mayo Clinic, Stanford University, University of Pittsburgh, Atrium Health and the list goes on and on. The CDC even setup a website to allow researchers to develop their own tests and to provide some general guidelines. While on the surface this seems smart, it also means we don’t have any national coordination in our Covid-19 testing on the ground.
The second type of test that is just now being release is a test to look for IgM and IgG antibodies in the blood of patients. You might remember in the previous post where I talked about us building immunity to the virus? Well, antibodies are one of the hallmarks of immunity, and we can test for them, even after we’re no longer infected. A simple prick of the finger (a little blood) on a indicator strip and we have a positive or negative for SARS-CoV-2 antibodies in minutes rather than hours or days, think of it like a pregnancy test for Coronavirus (United Biomedical, Aytu Bioscience). The problem with these tests is that SARS antibodies may not be detectable until 7-14 days after onset of symptoms (Chan et al 2005), so there’s a good chance they won’t identify people who are in the early stages of disease. They WILL help us dramatically as we attend to understand the true prevalence of the disease and how many people are now immune. Once a person is immune and recovered you’re very unlikely to pickup or spread the disease.
Drugs and Clinical Trials
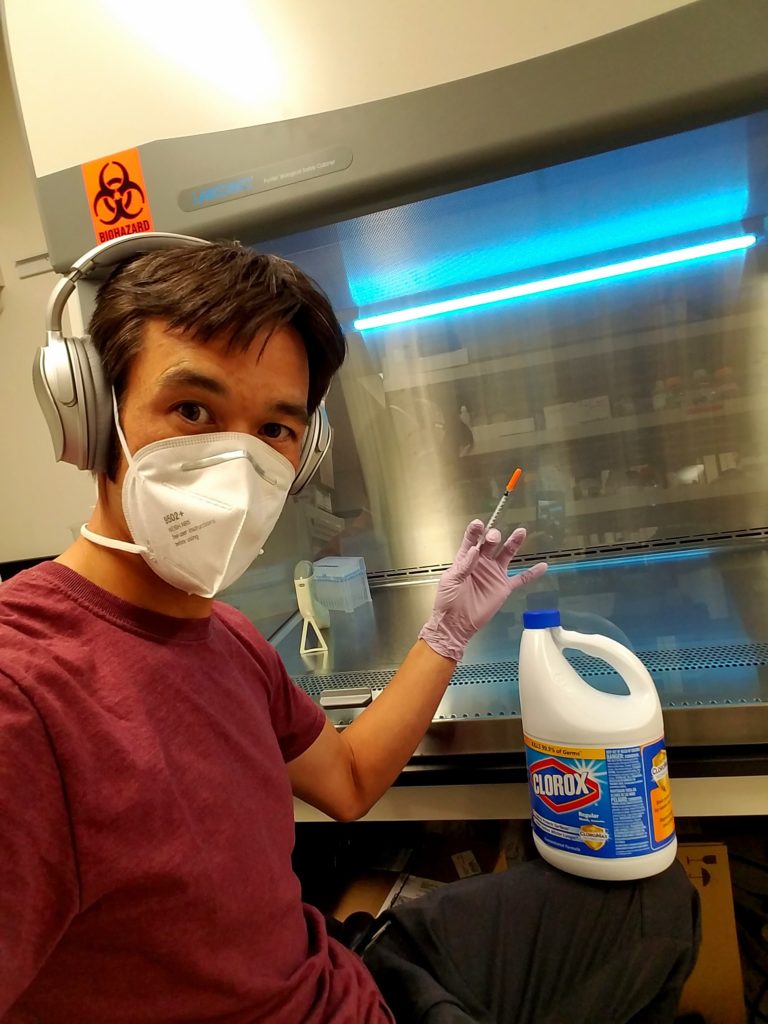
Much to the chagrin of many of us in the biomedical research sciences and healthcare, Donald Trump touted hydroxychloronquine as a ‘game changer’….wow wow, let’s pump the breaks for a second, back it up, and talk about the process by which drugs are created, rigorously tested and finally produced for mass distribution (if they even make it there). The first step is identifying potential drugs and targets then testing them in a laboratory to see if they actually work like you hoped and they’re not excessively toxic. This usually involves some mix of cell culture and animals models. If a candidate is lucky enough to make it through the lab testing phase (known as pre-clinical trials, only 1 in 1000 do) then the company can apply to the FDA to move it’s drug on to a multi-stage Clinical trial in human subjects. Phase I of the clinical trials process involves taking healthy individuals and dosing them with the new drug (usually starting low and escalating). They have to look for safety, effects on the body, toxicity, side effects, maximum tolerate dose, tissue distribution, half-life and on and on. IF the drug makes it through this initial phase then it’s on to Phase II where the drug is tested in a medium size group of diseased individuals (in this case Covid-19 positive). All of this under careful supervision of doctors who are specially trained to assess dosing and efficacy. If the drug proves efficacious in this Phase II study it will move on to a larger Phase III randomized double blind study where the drug being tested is compared to a placebo control (sugar pill) to ensure that it’s really the drug having an effect. These large studies can include 1000s of people and take many years depending on the nature of the disease being tested. Finally, once a drug survives Phase III; proving safe, efficacious and with the dosing amount and regimen worked out, the company can file for approval from the FDA (1 in 5000 make it this far)(medicine.net). This whole process can take up to 12 years for chronic diseases, but of course right now things are moving much more rapidly, and a lot of the regulations and paperwork are being modified to speed up the process.
So what about all the drugs that are being tested against Covid-19 right now? There are several drugs that were identified as being potential therapeutics, and thankfully they had already passed Pre-clinical testing and Phase I trials, so this dramatically expedites the process of testing. The most promising seem to be Remdesivir (from Gilead), Favipiravir (anti-viral), and the previously mentioned hydroxychloroquine (cdc.gov, Dong et al, Wang et al). Even though all of these drugs have successfully completed varying levels of clinical trials, using them against a new disease requires a new round of efficacy, dosing and safety testing. Patients with different diseases respond to drugs differently, dosing needs to be adjusted for the new disease and of course the drug needs to be thoroughly tested to ensure that the differences seen in early studies weren’t simply because of patient selection, population bias or other factors that were not controlled for with the small sample set. In short, all these drugs, while promising, are many months away from being approved for safe use in a wide array of Covid-19 patients, if they get there at all. See the comment below from my college friend Aileen, who’s a pharmacist in the San Francisco Bay Area in response to the small test of hydroxychloroquine in patients in France (Gautret et al)….
More PSA from a pharmacist….to detail out certain claims Hydroxychloroquine used in this case is in particular HIGH DOSE (usual dose of the drug is 200-400mg daily, in this case…600mg daily and we only use that dose in Q Fever patients). When the hydroxychloroquine in high dose and azithromycin are taken together, there are risks for GI side effects…and most importantly…POTENTIAL ARRHYTHMIA. First azithromycin is a known QT prolonging agent…but also…hydroxychloroquine can either cause direct mycocardial toxicity or exacerbate underlying mycocardial dysfunction. This is a RISK that must be weighed by physicians and healthcare professionals vs. the unproven benefits.
Is there promise? potentially….but we NEED MORE EVIDENCE TO EVALUATE SAFETY AND EFFICACY.
Please…do not demand for it….leave it to healthcare professionals to make that decision and do our jobs….
The next question is in regards to a vaccine against Covid-19. Unfortunately, the process I outlines above for drugs, also applies to vaccines, but we’re starting from ground zero. Prior to this pandemic there were no coronavirus vaccines available (though plenty of background research), so companies have gone into serious overdrive trying to develop something, and amazingly in just two months Moderna, in collaboration with the NIH, took the first vaccine candidate to Phase I clinical trials this month (March 2020) (nih.gov). A process that usually takes 6-12 months took them 2, let that sink in for a moment. And they’re not the only company working hard on creating a vaccine, as there are numerous others with vaccine designs being tested in Pre-Clinical trials as we speak. But, this bring us back to question of time. Before a vaccine can be deployed to the general public it has many hurdles to pass, and only if it successfully passes those hurdles can it be mass produced and distributed. So, as Dr Fauci has explained many times, we’re looking at best case 12-18months for a vaccine. Guess we’re going to have to hang tight and weather this storm for a bit longer.
Seasonality
Most people have probably heard the claim at one point or another that this thing (Covid-19) is like the flu and it’ll go away when the weather warms up. Even our President claimed “…you know, a lot of people think that (the virus) goes away in April with the heat — as the heat comes in. Typically, that will go away in April.” Is there any logic or scientific evidence to support this claim? The short answer is, no, but it’s definitely more complicated than that.
The idea of seasonality was brought up because the influenza virus does see a very seasonal pattern of spread and retraction. During the cooler winter months in the Northern Hemisphere we see a dramatic rise in influenza infection rates, then a drop as the weather warms in April, as Trump suggested. There are many reasons for this; reduced contact time between people (stuck inside, schools) as weather improves, improvements in immune responses due to people being outside more and increases in Vitamin D, potential increase in duration of infection during winter months, and decreased survival of some pathogens in warmer environments (Fisman et al). While we do have the first three things going for us as they are environmental changes that aren’t pathogen specific, what about the survival time of different viruses? It’s been well documented that influenza viruses survive and transmit best at lower environmental temperatures in the range of 5C and 20C. Though starting at 20C, depending on humidity, influenza virus transmission becomes much more variable, and at 30C a dramatic decrease is seen in viral transmission (Lowen et al). Unfortunately, coronaviruses don’t seem to have the same susceptibility profile. Testing on the original SARS-CoV-1 virus showed that it was fairly stable at environmental temperatures as high as 33C (91F), and only when temperature was increase to 38C (100F) did the virus infectivity begin to dramatically drop (Chan et al 2010). SARS-CoV-2, the causative agent of Covid-19 seems to be more temperature resistant than the influenza viruses that we commonly associate with having seasonal cycles. So with the virus currently spreading in the Southern Hemisphere and in several warm weather countries we shouldn’t expect too much help with the virus from Mother Nature’s change of seasons.
But not all hope is lost! I’ve heard recently that the extreme measures taken by many states have allowed the hospitals in the US a little breathing room. Even if this is short lived it means that staff and supplies can be replenished and that buys more time for widespread testing to come on line. Countries like Germany and South Korea are good case studies for how excellent testing and surveillance can lead to minimizing the number of fatalities (testing large percentages of their populations, and doing so quickly). Even though cases and number of deaths are still increasing, we’re slowly catching up on testing, and keeping our death rate low, but the fact that we have 2,122 serious or critical Covid-19 cases is still a little scary. For now, we’re all going to have to sacrifice a bit, be more compassionate to our fellow humans and just realize that we’re living through unprecedented times, that we will get through, though it’s going to take some time. If you’re interested in reading about some potential scenarios on how the pandemic plays out in the next 3-12months this article from the Atlantic outlines them pretty well in my opinion.
Citations
aytubio.com/covid-19/
cdc.gov/coronavirus/2019-ncov/hcp/therapeutic-options.html
Chan et al. The Effects of Temperature and Relative Humidity on the Viability of the SARS Coronavirus. Advances in Virology, 2011.
Chan et al. Serological response in patients with Severe Acute Respiratory Syndrome Coronavirus infection and Cross-Reactivity with Human Coronavirus 229E, OC43, and NL63. Clinical and Diagnostic Laboratory Immunology, 2005.
Dong et al. Discovering Drugs to treat Coronavirus disease 2019 (Covid-19). Drug Discoveries and Therapeutics, 2020.
Fisman et al. Seasonality of Viral Infections: mechanisms and unknown. European Society of Clinical Microbiology and Infectious Diseases, 2012.
Gautret et al. Hydroxychloroquine and azithromycin as a treatment for Covid-19: results of an open-label non-randomized clinical trial. Journal of Antimicrobial Agents, 2020.
Lowen et al. Roles of Humidity and Temperature in Shaping Influenza Seasonality. Journal of Virology, 2014.
nih.gov/news-events/news-releases/nih-clinical-trial-investigational-vaccine-covid-19-begins
unitedbiomedical.com/COVID-19/
Vincent et al. Chloroquine is a potent inhibitor of SARS coronavirus infection and spread. Virology Journal, 2005.
Wang et al. Remdesivir and chloroquine effectively inhibit the recently emerged novel coronavirus (2019-nCov) in vitro. Cell Research, 2020.
washingtonpost.com/world/2020/03/24/coronavirus-latest-news/
worldometers.info/coronavirus/